Leprosy Mailing List – March 13, 2020
Ref.: (LML) SDR-PEP and the risk of MB HD
From: Joe Almeida, London and Mumbai
Dear Pieter and colleagues,
Thanks to Khorshed Alam for his thoughtful comments on the review of SDR-PEP and the risk of MB HD (LML 5 March 2020). Does objective evidence bear out his views? LML enables such rapid, open discussion through which we can advance our understanding and boost our chances of permanently defeating the bacilli.
The review had agreed with Khorshed Alam's view that an exemplary HD (Hansen's disease) control programme has long been run in this part of Bangladesh. Household contacts, especially of infectious patients, are known to have a much higher risk of HD than other persons. In this rural health programme, all household contacts of newly diagnosed patients have been routinely examined since at least 1995. This was not a recently introduced feature. Household contact examination has long been intensive and prolonged (during years 0-2 following diagnosis in households with a new PB patient and years 0-5 in those with new MB patient). (1) This cannot explain the demonstrable retardation in the decline of HD in these 4 districts after 2010.
The sheer magnitude of the incidence rate, too, cannot explain the said retardation after 2010, because this magnitude was much greater in earlier years.
The overall intensity of active case-finding in the total population is indicated by objective evidence. As the frequency of active case finding increases, the total new patient detection rate increases. However, the proportion of MB HD among newly detected HD patients simultaneously decreases. This is because many single-lesion PB and other self-limiting forms of HD are revealed by more frequent active case-finding.
Figure 1. (based on ref 2) There is demonstrable inverse relationship between the intensity of active case-finding and the proportion MB among newly detected HD patients. For every 10% increase in the proportion of new patients detected by active case-finding, a 7.5% decrease was observed in the proportion of MB HD among newly detected cases
In this area of Bangladesh, the proportion of MB HD was reported to increase across 2010 and beyond. (3) This indicates a decrease in the overall intensity of active case-finding across the population. This tends to produce a fall in the number of new patients detected/yr, and cannot readily explain the levelling-off observed.
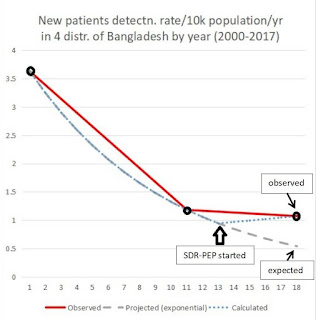
SDR-PEP was given to a substantial proportion of contacts of all newly detected MB HD patients in these 4 districts of Bangladesh in the MALTALEP trial. A population of 8 million with a new case detection rate of about 1 in 10,000/year including an MB proportion of about 25% is expected to yield only about 200 new MB patients/year. The MALTALEP trial included the contacts of 475 index MB patients. 7039 contacts received SDR-PEP, and 14988 contacts in total were included for BCG (re)vaccination. BCG alone was demonstrated to have some protective effect against all forms of HD by comparison to historical placebo-treated controls in this area, plus a strongly protective effect is demonstrable against MB HD. Despite this, SDR-PEP seemed to erase any favourable epidemiological impact at population level.
Figure 2. SDR-PEP produced no favourable epidemiological impact in the MALTALEP trial area, and may even have contributed to the retardation of the earlier decline.
In areas with less accomplished expertise, facilities, and operational capacity, the epidemiological impact of SDR-PEP is likely to be even less favourable. Such unfavourable impact is striking in itself, even if the risk of selecting drug-resistant mutant bacilli is ignored.
The risk of selecting drug-resistant mutants is brought on by the use of a single drug (rifampicin) instead of multi-drug chemoprophylaxis. The risk of selecting drug-resistant mutants is highest among missed LL patients in programmes that lack clinical expertise, skin smears, serology etc.. LL patients with few or no physical signs of disease are then liable to be misclassified as healthy contacts and given SDR-PEP. That is a recipe for the selection of drug-resistant bacilli. Even experienced clinicians have been known sometimes to miss the often subtle physical signs of early LL disease, when tens of millions of viable bacilli per day are still shed. (4) Minimally trained staff are almost certain to make this mistake.
Nevertheless, this is an exciting time in the history of public health because we can achieve near-zero transmission of HD once we focus on emulating success. A rapid decline of HD (17% to 20%/yr) was already demonstrated in Shandong and Uele at a time when they had a relatively low GDP per capita, as discussed here previously. Similar success can be spread across the globe. We are like detectives working out how the vicious criminals (the bacilli) operate and what impact is demonstrable from our efforts. We can keep discarding what does not work, expanding and improving what works.
Discussion of the example protocol for safe interruption of transmission indicated why HD continues to spread, and what we need to do in order to achieve zero transmission. Previously treated LLp patients with covert recurrent disease probably play an important role in Bangladesh, as they demonstrably do elsewhere.(5) They serve as enduring sources of concentrated viable bacilli. Past sequelae tend to disguise the recurrence of disease in such patients. The risk of new HD among their contacts remains high for years. Prolonged anti-microbial protection for LL patients, such as by post-MDT chemoprophylaxis with 3 bactericidal drugs, can not only protect the individual patient but also switch off this important source of concentrated viable bacilli. Esteemed colleagues, armed with the most helpful technology, can improve such example protocols and adapt them to their own areas. This might yield an even more rapid decline in HD than the 20%/yr achieved in Shandong and Uele.
Instead of HD being considered too trivial a problem to deserve attention, it can become a triumph of science-based intervention for zero transmission. Zero transmission is demonstrably within reach everywhere, except perhaps in the Americas where armadillos can maintain transmission. No child should develop HD. That is our shared dream, and it is demonstrably achievable. As we keep helping one another to spot critical clues and to focus on what works, we boost our chances of success. Drug resistance is the most important threat to our success, and the use of single drugs (eg., SDR-PEP) is the surest way to increase this threat. We know from the experience in TB that mathematical models are useless in the face of drug-resistance because drug-resistance is a discontinuity. It is more like falling off a cliff than gently sliding down a hillside.
Best wishes to Khorshed Alam and all who are working on HD. We are working together to save human nerves, limbs, eyes, minds, livelihoods, rights and relationships. We cannot afford to overlook clues, nor to fail, nor to leave our children a legacy of drug resistance and continued transmission of HD. Shandong succeeded. So can we, if we keep steering away from demonstrable failure and emulate demonstrable success instead
Joel Almeida
References
1. Butlin CR, Nicholls P, Bowers B et al. Household contact examinations: outcome of routine surveillance of cohorts in Bangladesh. Lepr Rev (2019) 90, 290–304
2. Xiang-Sheng Chen, Wen-Zhong Li, Cheng Jiang, & Gan-Yun Ye. Leprosy in China: epidemiological trends between 1949 and 1998. Bulletin of the World Health Organization, 2001, 79: 306–312
3. Butlin CR, Nicholls P, Bowers B et al.Outcome of late healthy household contact examinations in leprosy-affected households in BangladeshLepr Rev (2019) 90, 305 – 320
4. Davey TF, Rees RJ. The nasal dicharge in leprosy: clinical and bacteriological aspects. Lepr Rev. 1974 Jun;45(2):121-34.
5. Rao PS, Mozhi NM, Thomas MV. Leprosy affected beggars as a hidden source for transmission of leprosy. Indian J Med Res. 2000 Aug;112:52-5.
| | ||||
| | ||||
LML - S Deepak, B Naafs, S Noto and P Schreuder
LML blog link: http://leprosymailinglist.blogspot.it/
Contact: Dr Pieter Schreuder << editorlml@gmail.com
You received this message because you are subscribed to the Google Groups "Leprosy Mailing List" group.
To unsubscribe from this group and stop receiving emails from it, send an email to leprosymailinglist+unsubscribe@googlegroups.com.
To view this discussion on the web, visit https://groups.google.com/d/msgid/leprosymailinglist/ff8a8d5b-7a4d-471a-99b9-2178146edc1e%40googlegroups.com.

No comments:
Post a Comment